
Morton's Neuroma Surgery Success Rates: What to Know
Morton’s Neuroma can feel like you’re walking with a pebble stuck under your foot—except there’s nothing there. If you’re reading this, chances are you’ve been dealing with that burning, stabbing pain between your toes, and conservative treatments haven’t given you the relief you hoped for.
This is where surgery starts to feel like a real option. But before you take that step, you probably have a lot of questions: What are the success rates? Will surgery actually fix the problem for good? What if the pain comes back? These are all valid concerns, and that’s exactly what we’ll cover here.
Understanding the Morton’s Neuroma surgery success rates can help you make an informed decision. Whether you’re gathering information for yourself or a loved one, knowing what to expect—and what factors influence your outcome—can make all the difference.
Overview of Morton’s Neuroma Surgery
What Happens During Surgery?
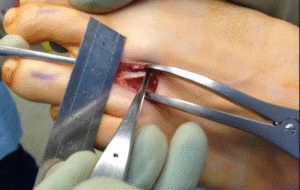
Morton’s Neuroma surgery is designed to relieve the pressure on the affected nerve—or remove it entirely if necessary. There are a few different surgical techniques, and the right one for you depends on factors like how long you’ve had symptoms and how severe they are.
Types of Surgery
- Neurectomy: This is the most common surgery. The surgeon removes the swollen nerve, aiming to stop the pain at its source.
- Decompression Surgery: Instead of removing the nerve, the surgeon creates more space around it by cutting nearby ligaments.
- Cryosurgery: A newer, minimally invasive option that freezes the nerve, stopping it from sending pain signals.
When is Surgery Recommended?
Surgery is usually considered after non-surgical best treatments—like orthotics, physical therapy, and injections—have failed. It’s not the first line of treatment, but for many people, it’s the only path to long-term relief when nothing else works.
Goals of Surgery
- Reduce or eliminate pain
- Restore your ability to walk comfortably
- Prevent the neuroma from getting worse
While surgery can be highly effective, it’s important to remember there are risks, and results can vary. That’s why understanding success rates and factors that affect them is crucial.
Defining “Success” in Surgery Outcomes
What does a “successful surgery” actually mean? Success isn’t just about the procedure itself—it’s about how well you recover, how much pain relief you get, and how much your daily life improves.
Success Isn’t One-Size-Fits-All
For some people, success means total freedom from pain. For others, it’s being able to walk a few miles without discomfort. That’s why it’s so important to set realistic expectations upfront.
Key Factors That Define Surgical Success
- Pain Relief: Most patients experience reduced or completely resolved pain after surgery. However, some may still feel minor discomfort.
- Return to Activities: A successful outcome often means getting back to walking, exercising, or even wearing regular shoes comfortably.
- Long-Term Relief vs. Short-Term Fix: True success is measured not just in the first few months but over several years. Some people feel great at first, only to have symptoms slowly creep back.
- Patient Satisfaction: Your own perception matters. If you feel your quality of life has improved and the surgery was worth it, that’s a success in itself.
Understanding these different angles of success can help you have realistic, informed conversations with your surgeon—and set the stage for a smoother recovery.
Reported Success Rates: What the Research Says
When you’re considering surgery for Morton’s Neuroma, one of the first things you want to know is—what are the success rates? After all, surgery is a big decision, and you want to feel confident that it’s worth it.
What the Data Tells Us
Several studies have tracked outcomes for people who undergo different types of Morton’s Neuroma surgery. While success rates vary depending on the specific procedure, research consistently shows that the majority of patients experience significant relief.
- Neurectomy (nerve removal): Studies report success rates between 75% to 85% within the first year after surgery. However, success rates tend to decline slightly over time if scar tissue or nerve regrowth occurs.
- Decompression surgery: This less invasive option offers initial success rates of about 70% to 80%, especially for early-stage neuromas. However, some cases may require follow-up treatment.
- Cryosurgery: While newer and not as widely studied, early reports show promising success rates around 80%, particularly when performed by experienced specialists.
Success Rates Are Not the Whole Story
Numbers only tell part of the story. Many studies define “success” as pain reduction, but patients often care about much more—like being able to walk comfortably or wear regular shoes again.
Factors That Complicate Research
It’s also important to know that success rates can vary depending on how studies are designed. Some factors that influence the numbers include:
- Length of follow-up (short-term vs. long-term results)
- How success is measured (pain scale vs. functional improvement)
- Patient selection (younger, healthier patients may have better outcomes)
Reported success rates are helpful, but they’re not guarantees. Your personal outcome depends on several factors—many of which are in your control.
Factors Affecting Surgical Success Rates
If you’ve been wondering why some people rave about their Morton’s Neuroma surgery while others regret it, the answer lies in these crucial factors affecting surgical success rates. Knowing what influences your chances can help you make smart choices—before, during, and after surgery.
1. Your Overall Health and Age
Younger, active patients without other foot problems often recover faster and more completely. If you have underlying issues like diabetes, poor circulation, or other foot deformities, your risk for complications rises.
2. The Severity and Duration of Your Neuroma
The longer you’ve had symptoms, the more complex the surgery can become. Early-stage neuromas often respond better to decompression, while long-standing, severe cases may require full nerve removal.
3. Your Surgeon’s Experience
Surgical outcomes improve when your surgeon specializes in foot and ankle procedures—especially nerve-related ones. Choosing a board-certified podiatrist or orthopedic surgeon with extensive experience treating Morton’s Neuroma directly improves your odds.
4. Post-Surgery Care and Compliance
Surgery itself is just part of the equation. Following your post-op instructions—like wearing proper footwear, avoiding high-impact activities, and doing any recommended rehab—can make or break your success.
5. Lifestyle and Footwear Choices
Even after surgery, some habits can set you back. Wearing narrow or high-heeled shoes, skipping orthotics, or ignoring foot pain could lead to recurrence or complications.
Pro Tip
Many patients who enjoy long-term relief take a proactive approach to foot health. Switching to supportive shoes, managing weight, and staying aware of early warning signs all play a role.
Surgical success isn’t just luck—it’s the result of preparation, smart choices, and ongoing care.
Risks and Complications After Surgery
Every surgery comes with risks, and Morton’s Neuroma surgery is no exception. The good news? Most complications are rare when you work with an experienced surgeon. Still, it’s important to know what could go wrong—so you can make an informed decision and take steps to lower your risk.
Common Post-Surgery Risks
- Infection: As with any surgery, there’s a small chance of infection at the incision site.
- Swelling and Bruising: This is normal after foot surgery but should gradually improve over a few weeks.
- Delayed Healing: Certain health conditions (like diabetes or poor circulation) can slow the healing process.
Potential Long-Term Complications
- Stump Neuroma: In cases where the nerve is removed, a small bundle of nerve tissue can regrow at the surgical site, causing new pain.
- Numbness or Tingling: Depending on how much nerve tissue is involved, some patients experience permanent numbness between the toes.
- Chronic Pain: While rare, some patients develop complex regional pain syndrome (CRPS)—a nerve-related pain condition that can be challenging to treat.
Recurrence—Can It Come Back?
One of the biggest fears patients have is, “What if the neuroma comes back?” In some cases, scar tissue or nerve regrowth can trigger symptoms again. This is why following post-surgery advice—and wearing the right shoes—matters so much.
Minimizing Your Risk
- Choose an experienced surgeon
- Follow post-op care instructions carefully
- Use orthotics if recommended
- Avoid high-heeled, narrow shoes
- Stay active, but avoid high-impact exercise until fully healed
While understanding risks and complications after surgery can feel overwhelming, being informed puts you in control. The better prepared you are, the smoother your recovery—and the better your chances of long-term success.
How Success Rates Compare to Non-Surgical Treatments
If you’re unsure about surgery, you’re not alone. Most people with Morton’s Neuroma start with non-surgical treatments—and for good reason. Surgery comes with risks, recovery time, and no absolute guarantee. So how do success rates for surgery really stack up against non-surgical options?
Non-Surgical Options: What’s Available?
Before surgery, most doctors recommend trying these conservative treatments:
- Orthotics: Custom insoless to relieve pressure on the nerve.
- Corticosteroid Injections: Reduce inflammation and pain.
- Physical Therapy: Helps improve foot mechanics.
- Alcohol Sclerosing Injections: A chemical injection that shrinks the nerve.
- Shockwave Therapy: Uses sound waves to break up scar tissue and reduce pain.
Success Rates for Non-Surgical Treatments
Studies show that non-surgical options help about 50% to 60% of people with Morton’s Neuroma. The catch? Relief is often temporary, and symptoms may return if you resume wearing tight shoes or high heels.
- Injections offer faster relief but may only last a few months.
- Orthotics and footwear changes work well for mild cases but are less effective for advanced neuromas.
Comparing Non-Surgical and Surgical Outcomes
Surgery has higher success rates—typically 70% to 85%—especially for patients who have had symptoms for years or who didn’t respond to conservative care. However, surgery requires recovery time, and there’s a small risk of complications like nerve regrowth (stump neuroma).
So Which Should You Choose?
It depends on your goals. If you want to avoid surgery and your symptoms are still manageable, non-surgical treatments are worth trying first. But if pain limits your daily life—and you’ve exhausted conservative options—surgery offers a better chance at long-term relief.
Patient Perspectives on Surgery Success
What does “success” really mean to you? For surgeons, success might mean removing the neuroma. But for patients, success is often about regaining a sense of normal life—walking without pain, wearing shoes comfortably, or enjoying favorite activities again.
Success Means Different Things to Different People
Some patients say surgery was life-changing. They went from limping through grocery stores to walking miles without pain. Others feel that while surgery reduced pain, it didn’t completely restore comfort, especially when wearing fashionable shoes.
What Patients Often Care About Most
- Pain Relief: Did the stabbing, burning pain go away—or at least improve enough to live with?
- Foot Function: Can they walk, exercise, or stand for long periods without issues?
- Footwear Freedom: Are they stuck in orthopedic shoes forever, or can they wear regular shoes again?
- Scar and Sensation: Is there numbness or tenderness around the scar?
Realistic vs. Ideal Outcomes
Many patients hope for a perfect foot after surgery—but that’s not always realistic. The nerve itself may be gone, but scar tissue, altered sensation, or mild stiffness can remain. The most satisfied patients tend to be those with realistic expectations going in.
What Successful Patients Have in Common
- They chose an experienced surgeon who explained all risks and benefits honestly.
- They followed post-surgery instructions closely.
- They adjusted their footwear habits permanently to avoid recurrence.
- They measured success by improved quality of life—not just by total elimination of symptoms.
Hearing patient perspectives on surgery success helps set realistic expectations—and reminds you that success isn’t always about perfection. It’s about progress.
Tips for Improving Your Own Success Rate
Whether you’re already scheduled for surgery or just starting to consider it, there are steps you can take to improve your own success rate. The good news? Many of these are within your control.
1. Choose the Right Surgeon
Experience matters. Seek a podiatrist or orthopedic surgeon who specializes in nerve-related foot surgeries—and who has treated plenty of Morton’s Neuroma cases specifically. Don’t be afraid to ask about their success rates.
2. Prepare Before Surgery
- Maintain a healthy weight (extra weight adds foot pressure).
- Stop smoking (it slows healing).
- Review your medications with your doctor to avoid complications.
3. Follow Post-Op Instructions
This is one of the biggest predictors of success. Stick to your recovery plan—wear your surgical shoe, avoid high-impact activities, and follow your doctor’s timeline for returning to regular shoes.
4. Invest in Proper Footwear
Even after surgery, the wrong shoes can trigger recurrence or discomfort. Choose shoes with:
- Wide toe boxes
- Cushioned soles
- Low, stable heels (under 1 inch)
5. Stay Active—but Smart
Once healed, gentle exercises like walking, swimming, or cycling can help restore strength and flexibility. Avoid high-impact sports (like running on hard pavement) until fully cleared by your doctor.
6. Watch for Early Warning Signs
Some people experience minor tingling or mild pain months after surgery. Don’t ignore it. Early intervention—like adjusting footwear or adding orthotics—can prevent bigger problems down the road.
Proactive Patients Have the Best Outcomes
The bottom line? Surgery can be a highly effective solution for Morton’s Neuroma, but it’s not a passive fix. Your actions—before, during, and after—play a huge role in your long-term success.
Recent Posts
Morton’s Neuroma Surgery Success Rates: What to Know
Morton’s Neuroma Surgery Success Rates: What to Know Morton’s Neuroma can feel like you’re walking with a pebble stuck under
