
How Painful is Morton's Neuroma Surgery?
If you’re dealing with the sharp, burning pain of Morton’s Neuroma, you’ve probably explored every option to find relief. From changing your shoes to trying injections, it can feel frustrating when nothing truly works.
At some point, surgery might come up as a solution—but with surgery comes a new concern: How painful is Morton’s Neuroma surgery, and what is recovery really like?
This guide is here to answer exactly that. Whether you’re anxious about the pain, unsure about the process, or simply want to know what to expect, you’re in the right place. We’ll break down the surgery, the pain involved, and the recovery process in a way that’s clear, honest, and easy to follow.
Understanding Morton’s Neuroma Surgery
What is Morton’s Neuroma Surgery?
Morton’s Neuroma surgery is a procedure designed to relieve the painful nerve compression between the toes, usually the third and fourth toes. This condition develops when the nerve becomes thickened and inflamed due to repeated pressure or irritation, often from tight shoes, high heels, or certain foot structures.
Surgery is typically considered when conservative treatments—like custom orthotics, corticosteroid injections, or physical therapy—no longer provide relief.
Types of Morton’s Neuroma Surgery
There’s no one-size-fits-all surgery for Morton’s Neuroma. Depending on the severity and location of your neuroma, your surgeon may recommend one of these approaches:
- Neurectomy (Nerve Removal)
In this procedure, the affected nerve is removed entirely. It’s highly effective for pain relief, but can lead to permanent numbness in the toes. - Decompression Surgery
This method aims to relieve pressure by cutting nearby ligaments. It’s a less invasive option and preserves the nerve, but isn’t always successful for severe cases. - Cryogenic Neuroablation
Although technically not open surgery, this minimally invasive technique freezes the nerve to stop pain signals. It’s often an outpatient procedure with a shorter recovery time.
When is Surgery Recommended?
Surgery isn’t the first step for Morton’s Neuroma. Most podiatrists will suggest surgery only if:
- You’ve had persistent pain for over 6-12 months.
- Non-surgical treatments (like orthotics, footwear changes, or injections) failed.
- Walking, standing, or wearing normal shoes has become unbearable.
Risks and Benefits of Surgery
Benefits:
- Long-term relief from burning and stabbing pain.
- Improved ability to walk, exercise, and wear normal shoes.
Risks:
- Persistent numbness in the toes.
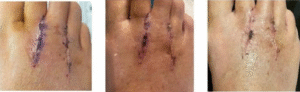
- Scar tissue formation.
- In rare cases, the neuroma may regrow, causing recurring pain.
Understanding these factors helps you make an informed decision, so you know what to expect and can weigh the trade-offs.
Pain During Morton’s Neuroma Surgery
What Happens During Surgery?
One of the biggest concerns people have is whether the surgery itself is painful. The good news? You won’t feel pain during the procedure because anesthesia is used.
Depending on the complexity of your case, your surgeon may use:
- Local Anesthesia: Numbs only your foot. You’re awake but feel no pain.
- Regional Anesthesia: Blocks sensation in the entire lower leg.
- General Anesthesia: You’re asleep throughout the surgery. This is less common for Morton’s Neuroma.
Is the Procedure Painful?
The surgery itself is painless, thanks to anesthesia. However, some patients feel mild pressure or tugging sensations if only local anesthesia is used. This isn’t painful—just a bit strange.
The real concern is post-surgery pain, which varies depending on factors like:
- The type of surgery you had.
- Your personal pain tolerance.
- How well you follow aftercare instructions.
What to Expect Immediately After Surgery
Once the anesthesia wears off, it’s normal to feel some soreness, throbbing, or swelling around the surgical site. This pain is manageable with:
- Prescribed pain medications.
- Over-the-counter pain relievers (like ibuprofen).
- Ice packs and elevation to reduce swelling.
Most people find the first 48 hours are the most uncomfortable—but the pain gradually decreases as healing begins.
Immediate Post-Surgery Pain and Discomfort
What to Expect in the First 24 Hours
The hours right after your surgery can feel overwhelming, especially if you’re unsure how painful things will be. Once the anesthesia wears off, you’ll likely notice some throbbing, soreness, and swelling in your foot. This is completely normal — your body is responding to the trauma of surgery.
Many people describe the pain as a deep ache, similar to a badly sprained ankle, with some added sharpness around the incision site. While this might sound intimidating, it’s temporary and manageable with the right care.
How Pain is Managed After Surgery
Your surgeon will provide a pain management plan tailored to your case. This usually includes:
- Prescription pain medication, especially for the first 48 hours.
- Over-the-counter options like ibuprofen (Advil) or acetaminophen (Tylenol) after the stronger meds taper off.
- Elevation and ice packs to reduce swelling, which also helps ease the pain.
It’s important to follow these instructions closely. The first day or two is when discomfort peaks — but many patients say that staying ahead of the pain (taking medication on schedule rather than waiting for pain to spike) makes all the difference.
Common Concerns: Is This Normal?
Here are some sensations you might experience:
- Tingling or numbness around the toes (due to nerve manipulation).
- A tight feeling across the ball of your foot.
- Increased pain when putting your foot down, thanks to blood rushing to the area.
These sensations are all typical in the first day or two. However, if your pain suddenly worsens, your foot feels unusually warm, or you notice redness spreading up your leg, contact your surgeon immediately — these could be signs of infection.
First Week of Recovery: Pain and Healing
How Pain Changes Over the First Few Days
Most patients find that the first 48 hours are the most challenging. After that, the sharp pain gradually eases into a dull ache, and swelling starts to improve. By day 4 or 5, you may notice the pain becomes more intermittent, triggered mainly by movement rather than constant discomfort.
What Activities Are Safe During the First Week?
Your foot needs time to heal, so expect to stay off your feet as much as possible for the first week. Short trips to the bathroom or kitchen are fine, but prolonged standing or walking can increase pain and swelling.
Some surgeons recommend using crutches or a knee scooter to keep pressure off your foot. Others might allow limited weight-bearing if your surgery was minimally invasive. Either way, trying to “push through the pain” or rushing recovery can set you back significantly.
Wound Care and Swelling Control
Good wound care not only prevents infection but also reduces unnecessary pain. Here’s what to focus on:
- Keep the dressing clean and dry — avoid getting it wet in the shower.
- Elevate your foot above heart level whenever you’re sitting.
- Use ice packs (wrapped in cloth) for 15-20 minutes every few hours to control swelling.
Emotional Side of Recovery
Pain isn’t just physical — it’s also frustrating and draining. It’s normal to feel impatient or discouraged, especially if you’re someone who’s always on the go. Remember, this first week is the foundation for your recovery, so giving your foot the rest it needs now will help you heal faster overall.
Weeks 2-6: Pain Progression and Mobility Improvement
How Pain Evolves During This Phase
By the second week, many patients notice that pain becomes much more manageable. Instead of sharp surgical pain, you’ll probably feel more of a stiff, sore sensation, especially after periods of rest. This is because your body is starting to form scar tissue, and the surrounding muscles and tendons are adjusting to the absence of the neuroma.
When Can You Start Walking Again?
This depends on your specific procedure and how well your healing progresses. In general:
- Week 2-3: Gradual weight-bearing in a surgical shoe may begin.
- Week 4: Some patients transition into loose, supportive footwear with soft soles.
- Week 6: Light walking is usually possible, but standing for long periods can still cause discomfort or swelling.
Physical Therapy and Exercises
Many podiatrists recommend gentle exercises to restore flexibility in the foot and prevent stiffness. These might include:
- Toe stretches (gently moving toes up and down).
- Ankle circles to keep circulation flowing.
- Calf stretches to relieve tension in the lower leg.
Physical therapy can also help if you’re struggling with balance or gait changes after surgery.
Dealing with Lingering Discomfort
It’s common to still feel occasional tingling, numbness, or mild aching even at the 6-week mark. This doesn’t necessarily mean something is wrong — nerves take time to heal, and your foot is still adjusting to its new normal.
That said, if pain suddenly worsens or you have trouble bearing weight at all, contact your surgeon for a follow-up evaluation.
Long-Term Recovery: Pain and Sensation Changes
What to Expect After the First Few Months
Once you’re past the initial recovery phase, you’ll start noticing subtle changes in how your foot feels. For many people, the sharp pain they lived with before surgery is gone—but that doesn’t always mean your foot feels completely “normal.”
Some lingering soreness, stiffness, or numbness is common, especially around the incision site or the toes. This is part of the nerve healing process, which can take several months—or even up to a year—for full sensation to settle.
Nerve Regeneration and Sensory Changes
Since Morton’s Neuroma surgery often involves removing or decompressing a nerve, your foot may feel different than it did before. You might experience:
- Tingling or pins-and-needles sensations as nerves regenerate.
- Numbness in the toes, especially after a neurectomy.
- Temperature sensitivity — some patients feel coldness or warmth more intensely than before.
These changes can feel strange, but they often improve over time. Your body is incredibly adaptable, and with gentle movement and proper footwear, your foot can regain both comfort and function.
When Will You Be Completely Pain-Free?
This is one of the most common questions—and the honest answer is, it varies. Some people feel back to normal within 3-4 months, while others experience minor aches or numbness for up to a year.
The key factors influencing your timeline include:
- The type of surgery you had (nerve removal tends to have longer-lasting numbness).
- How closely you followed post-surgery care.
- Your overall health and healing ability.
Patience is essential. Many patients feel discouraged when pain lingers longer than expected—but gradual improvement is completely normal in nerve-related surgeries.
Potential Complications and Chronic Pain Issues
Common Complications After Morton’s Neuroma Surgery
While most people recover well, it’s important to understand what could go wrong, so you can catch issues early. Some potential complications include:
- Scar tissue formation: This can press on nearby nerves, creating a new source of pain.
- Infection: Redness, warmth, and increasing pain could signal infection, especially in the first few weeks.
- Neuroma recurrence: In rare cases, the nerve stump may develop into a stump neuroma, essentially forming a new painful mass.
Chronic Pain After Surgery: Why It Happens
Although surgery is designed to relieve neuroma pain, a small percentage of patients experience persistent or chronic pain afterward. This could be due to:
- Incomplete removal of the damaged nerve.
- Nerve damage during surgery.
- Overactive nerve endings sending abnormal pain signals (a phenomenon known as neuropathic pain).
How to Know If Something’s Wrong
It’s normal for some aching, tingling, or tightness to last for months—but severe, stabbing pain or increasing discomfort long after surgery may indicate a problem. If you experience:
- Pain that’s getting worse instead of better.
- A burning sensation spreading beyond the surgery site.
- Difficulty walking even after several months.
It’s time to contact your podiatrist or surgeon for a thorough evaluation.
Tips for a Smooth Recovery
Set Yourself Up for Success from Day One
Recovery starts the moment you leave the operating room—and how you care for your foot in the early weeks plays a big role in your long-term comfort.
Follow These Core Principles:
- Stay ahead of the pain: Don’t wait for severe pain before taking medication.
- Elevate your foot: This reduces swelling and pressure.
- Rest, but don’t stay completely still: Gentle movement helps circulation and prevents stiffness.
Choose the Right Footwear
Your shoes matter more than ever after surgery. In fact, wearing the wrong shoes could undo some of the benefits of surgery. Post-recovery shoes should:
- Offer plenty of toe room.
- Have a soft, cushioned sole.
- Provide arch support to distribute pressure evenly.
Avoid:
- Tight shoes (especially pointed or narrow styles).
- High heels (which shift weight onto the ball of your foot).
Gradual Return to Activity
It’s tempting to jump back into your regular routine once pain improves—but pushing too hard can prolong swelling or cause setbacks. Ease back into activity with:
- Short, gentle walks on soft, flat surfaces.
- Light stretching to keep your toes and ankle flexible.
- Activities like swimming or cycling, which are low-impact.
Listen to Your Body
Every foot heals at its own pace. Some soreness is normal—but sharp or worsening pain is a red flag. Be patient, follow your podiatrist’s advice, and trust your body’s signals.
Stay Positive (and Realistic)
Surgery is a journey, not a quick fix. While many patients experience significant pain relief, no surgery guarantees perfection. Realistic expectations—combined with good aftercare—will help you get the best possible outcome.
Patient Experiences and Pain Levels
Every Patient’s Pain Experience is Different
If you’re considering Morton’s Neuroma surgery, one of the biggest questions on your mind is probably, “How much will it hurt?” The honest answer is that pain levels vary from person to person.
Some patients describe the pain as mild and manageable, while others go through a more challenging recovery period with discomfort lasting several weeks. Your experience will depend on:
- The type of surgery performed (neurectomy vs. decompression).
- Your personal pain tolerance.
- How well you follow post-surgery care guidelines.
Common Themes in Patient Stories
While every recovery journey is unique, many patients report similar patterns when it comes to pain and healing:
- First 48 hours: Pain peaks as anesthesia wears off, but medication and elevation help manage it.
- First week: Most describe pain as dull, throbbing, or tender, especially when standing or walking.
- Weeks 2-4: Discomfort gradually improves, but swelling or stiffness can linger if you overdo activity.
- After 6 weeks: Many patients start to feel significantly better, with occasional soreness after long walks or standing.
Real-Life Patient Insights
Reading real patient experiences can give you a clearer picture of what to expect. Here’s how some describe their recovery:
“I was nervous about the pain, but it was more of a deep ache than sharp pain. Staying ahead with pain meds and icing made all the difference.”
“The first week was tough, but by the third week, I was walking with just slight tenderness.”
“I still have a bit of numbness months later, but the burning pain I had before surgery is gone—and that’s a relief.”
These stories show that while the recovery process isn’t pain-free, most patients find the post-surgery pain far more manageable than the nerve pain they lived with before.
Factors That Influence Your Pain Level
Several factors play a role in how much pain you feel after surgery:
- Your overall health and healing speed.
- Pre-existing foot issues (like arthritis or flat feet).
- How closely you follow your surgeon’s recovery advice.
- The skill and technique of your surgeon.
Conclusion
Surgery is a Journey—But Relief is Possible
If you’ve been living with the stabbing, burning pain of Morton’s Neuroma, surgery can feel like a last resort—and it’s natural to worry about the pain involved. While no surgery is completely painless, many patients find that post-surgical discomfort is much easier to manage than the chronic nerve pain they had before.
What You Can Expect Moving Forward
By understanding what’s normal during recovery, you can feel more confident and prepared. Here’s a quick recap:
- Initial pain is temporary and manageable with proper care.
- Most patients feel significant improvement by the 4 to 6-week mark.
- Some numbness, stiffness, or mild aches may linger—but they’re typically far less disruptive than neuroma pain.
Trust the Process (and Your Body)
Recovery isn’t always linear—but if you listen to your body, follow your surgeon’s advice, and give yourself time to heal, you have every reason to expect a positive outcome.
If you’re still on the fence about surgery, talking to patients who’ve been through it or scheduling a consultation with a trusted podiatrist can help you make an informed, confident decision.
Recent Posts
How Painful is Morton’s Neuroma Surgery? Recovery Explained
Add Your Heading Text Here Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis,
