
When is Surgery Needed for Morton's Neuroma?
If you’ve been struggling with persistent foot pain, especially in the ball of your foot, you may have already heard of Morton’s neuroma. It’s a common yet frustrating condition that can make every step uncomfortable.
But when does this condition need surgery? Is it possible to avoid surgery altogether? These are the questions many people ask after months of trying to manage their symptoms.
In this guide, we’ll walk you through everything you need to know—starting from what Morton’s neuroma actually is to how doctors diagnose it, and ultimately, the key indicators that show surgery might be the best option for you.
Understanding Morton’s Neuroma
What Exactly is Morton’s Neuroma?
Morton’s neuroma is a thickening of the tissue around the nerves leading to your toes—most often between the third and fourth toes. This thickened tissue compresses the nerve, leading to pain, tingling, or a burning sensation.
What Causes It?
There isn’t always a single cause, but several factors can put extra pressure on the forefoot, such as:
- Wearing tight or high-heeled shoes
- Participating in high-impact sports like running
- Having foot deformities such as flat feet, bunions, or hammertoes
Symptoms You Shouldn’t Ignore
Morton’s neuroma symptoms often start gradually but worsen over time if untreated. The most common complaints include:
- A feeling like you’re standing on a pebble or fold in your sock
- Sharp, burning pain in the ball of the foot
- Numbness or tingling in the toes
Why It Matters
Ignoring these symptoms can lead to long-term nerve damage, making treatment more difficult. That’s why understanding your condition early—and knowing when to escalate to more serious treatments—is critical.
Diagnostic Process
Step 1: Clinical Examination
Your journey to diagnosis usually starts with a physical exam. A foot specialist will press on the area between your toes to check for tenderness, a telltale “clicking” sensation (Mulder’s click), or reproduction of your pain.
Step 2: Reviewing Your Symptoms and History
Your doctor will ask questions like:
- When did the pain start?
- What makes it better or worse?
- What kind of shoes do you normally wear?
- Do you participate in sports that stress your feet?
This conversation helps connect the dots between your lifestyle and your symptoms.
Step 3: Imaging Tests
If needed, your doctor may order tests to rule out other conditions like stress fractures or arthritis. The most common imaging options are:
- Ultrasound: Shows soft tissue thickening around the nerve.
- MRI: Provides detailed images to confirm nerve enlargement.
Why an Accurate Diagnosis Matters
Some foot conditions mimic Morton’s neuroma, from capsulitis to metatarsalgia, so accurate diagnosis ensures you get the right treatment plan. Surgery isn’t even on the table until all other causes have been ruled out—and only if your pain continues despite trying conservative treatments.
Conservative Treatments and Their Role
If you’ve recently been diagnosed with Morton’s neuroma, surgery might sound intimidating. The good news is, surgery isn’t the first step in treatment—and for many people, it’s not needed at all.
Conservative treatments are non-surgical options designed to ease your symptoms and help you walk comfortably again. They focus on reducing pressure on the nerve, calming inflammation, and improving how your foot functions.
Footwear Modifications: Small Change, Big Impact
The shoes you wear play a major role in either relieving or worsening your pain. Narrow or high-heeled shoes squeeze the bones of your foot together, trapping the nerve between them.
Switching to wide, supportive shoes with low heels and plenty of cushioning can significantly reduce pressure on the affected nerve. Many people see real improvement with this one simple change.
Custom Orthotics and Padding
If changing your shoes isn’t enough, custom orthotics—specially made inserts that support your arch and redistribute weight—can help. Padding placed near the ball of your foot can also lift and separate the bones, reducing nerve compression.
Physical Therapy
A skilled physical therapist can guide you through stretches and exercises to ease tension in your foot and improve alignment. In some cases, poor foot mechanics contribute to nerve compression, and addressing that can provide lasting relief.
Medications and Injections
- Anti-inflammatory medications (like ibuprofen) can reduce swelling around the nerve.
- If pain is more severe, your doctor may suggest corticosteroid injections, which deliver targeted relief directly to the problem area.
Why Conservative Care Matters
Conservative treatments allow you to stay active while addressing the root cause of your symptoms. They’re also far less risky than surgery. Most experts recommend trying these approaches for several months before even considering surgery (source: American Orthopaedic Foot & Ankle Society).
When Conservative Treatments Fail
How Do You Know It’s Time to Re-evaluate?
For many people, conservative treatments bring relief—but not always. If you’ve given these options a fair try (typically 3-6 months) and your pain is still interfering with daily life, it may be time to explore other options.
Key Signs That Conservative Care Isn’t Working
- Ongoing pain despite footwear changes and orthotics
- Temporary relief from injections—but pain always returns
- Symptoms are getting worse over time
- You’ve had to significantly limit your activity to avoid pain
What’s Next?
When non-surgical care doesn’t bring enough relief, it’s natural to feel frustrated—or even worried about what comes next. This is where a thorough reassessment with your foot specialist becomes essential.
They’ll review your symptoms, check for any changes on imaging, and talk through the pros and cons of surgery or alternative treatments. Many people feel reassured when they realize that surgery, when needed, can be extremely effective at providing lasting relief.
Key Indicators That Surgery May Be Needed
Surgery Isn’t the First Step—But Sometimes It’s the Right One
The decision to have surgery for Morton’s neuroma isn’t made lightly. Most doctors recommend surgery only after conservative treatments have failed and your quality of life is suffering.
If you’re wondering whether you’ve reached that point, here are key indicators that surgery may be the next logical step:
1. Severe, Persistent Pain Despite Treatment
If you’ve diligently followed all the recommended treatments—changed shoes, tried orthotics, completed physical therapy, and even had injections—but the pain still limits your daily activities, surgery may offer the lasting relief you need.
2. Pain Is Limiting Your Mobility and Lifestyle
Are you avoiding walks, skipping workouts, or even limiting social activities because of foot pain? When pain starts controlling your life, it’s a clear sign that more aggressive treatment might be necessary.
3. Imaging Shows Progressive Changes
If follow-up imaging (like ultrasound or MRI) shows that the neuroma is getting larger or that the tissue is thickening even more, this can indicate that the nerve is under constant stress. Surgery may be the best way to remove the source of pain before it worsens further.
4. Recurrent Symptoms After Temporary Relief
Some people find relief with steroid injections, but if the pain keeps coming back and the relief periods are getting shorter, that’s a strong sign that injections are only masking the underlying problem, not solving it.
5. You Want a Long-Term Solution
If you’ve been managing symptoms for years and feel like you’re stuck in an endless cycle of flare-ups and treatment, surgery can offer a more definitive solution. While no procedure guarantees perfection, many patients experience significant, lasting relief after surgery.
What Surgery Can—and Can’t—Do
Surgery can remove or decompress the nerve, resolving the mechanical compression causing your pain. However, it does come with risks like numbness in the toes or possible recurrence of symptoms.
This is why it’s so important to work closely with a foot specialist who understands your specific goals—whether that’s returning to high-impact sports or simply being able to walk comfortably again.
Types of Surgical Options for Morton’s Neuroma
When conservative treatments have failed and your pain is affecting your quality of life, your doctor might suggest surgery for Morton’s neuroma. Surgery can sound daunting, but understanding your options can help you feel more confident about your decision.
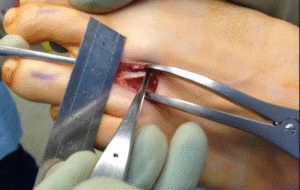
Neurectomy: Removing the Problem Nerve
This is the most common surgery for Morton’s neuroma. In a neurectomy, the surgeon removes the thickened, damaged nerve between your toes. Without the nerve, the pain signals stop—but this also means you may experience some permanent numbness in the affected toes.
For many people, this trade-off is worth it if it means they can walk without pain again. According to research published in The Journal of Foot and Ankle Surgery, neurectomy success rates range between 75% to 85%, making it a reliable option when non-surgical treatments fail.
Nerve Decompression: Relieving Pressure Without Removing the Nerve
Some surgeons prefer a less aggressive approach—nerve decompression. Instead of removing the nerve, the surgeon releases the tight ligaments or tissue that’s pressing on it. This preserves the nerve and reduces the risk of numbness.
This technique may be more suitable if your neuroma is smaller or caught earlier. However, for chronic cases where the nerve is severely damaged, decompression might not offer long-term relief.
Open vs. Minimally Invasive Surgery
Both neurectomy and decompression can be done using either:
- Open surgery: A larger incision for direct access to the nerve.
- Minimally invasive surgery: Tiny incisions with specialized tools and sometimes a camera for guidance.
Minimally invasive techniques may offer faster recovery and less scarring, but they aren’t always suitable for larger neuromas. Your foot surgeon will recommend the approach that best fits your situation.
Risks and Benefits of Surgery
It’s natural to feel hesitant about foot surgery. Understanding both the potential benefits and the risks helps you make an informed choice.
What You Stand to Gain
- Significant pain relief: For most people, surgery successfully removes or relieves nerve pressure, offering lasting relief.
- Return to normal activity: Many patients can resume walking, sports, and daily routines once healing is complete.
- Permanent fix for some: When the nerve is removed, the source of the pain is gone for good.
What You Need to Consider
- Numbness: If the nerve is removed, the space between your toes may feel permanently numb. While this is usually not bothersome, it’s important to know.
- Scar tissue formation: In some cases, the healing process can create scar tissue that irritates the surrounding area—a condition called stump neuroma.
- Incomplete relief: While surgery helps the majority of patients, about 15-20% still experience some degree of pain afterward, especially if there are other underlying foot issues (like poor foot mechanics or arthritis).
Personal Factors That Affect Your Risk
- Your overall health (diabetes, poor circulation, or smoking can slow healing)
- Your activity level (athletes may need special recovery plans)
- Previous foot surgeries or chronic foot deformities
The Bottom Line
Surgery is a tool—not a magic fix. But when conservative care isn’t enough, it can give you back the ability to walk, move, and live without constant pain. Many patients say they wish they hadn’t waited so long to explore it.
Post-Surgery Recovery and Long-Term Outlook
If you’re considering surgery, you’re probably wondering: How long will recovery take? and What should I expect after surgery? Let’s break it down into clear phases so you can prepare confidently.
Immediate Post-Surgery: The First Few Days
After surgery, your foot will be bandaged and possibly in a surgical shoe to protect the area. You’ll need to keep your foot elevated and avoid putting weight on it for at least a few days.
Mild pain, swelling, and bruising are completely normal, and your doctor will recommend pain medication to keep you comfortable.
Early Healing: Weeks 1-3
You’ll gradually transition to walking short distances, often with the help of crutches or a walker. Many patients can wear comfortable, wide shoes after about 2-3 weeks, but high-impact activities are off-limits for a bit longer.
Full Recovery Timeline
- Walking comfortably: 4-6 weeks
- Return to most daily activities: 6-8 weeks
- High-impact sports or running: Around 3 months (or more, depending on healing)
Recovery speed varies from person to person. Factors like your age, weight, overall health, and how well you follow post-op care all play a role.
What Long-Term Results Can You Expect?
The good news is that the majority of patients experience substantial or complete pain relief after surgery. In fact, studies show that 80% or more of patients are satisfied with their outcome (source: Foot and Ankle International Journal).
However, some may notice:
- Mild numbness between the toes (usually not bothersome)
- Occasional stiffness if scar tissue forms
- Need for ongoing footwear adjustments to prevent new foot issues
Tips for Long-Term Foot Health
- Stick with supportive, well-cushioned shoes
- Use custom orthotics if your foot shape or gait needs correction
- Avoid repetitive stress from high-impact sports if possible
Special Considerations
Every foot is unique, and so is every case of Morton’s neuroma. Before deciding on surgery, it’s important to consider factors that could affect your outcome, recovery, and long-term comfort.
Your Overall Health and Medical History
If you have diabetes, poor circulation, or nerve conditions like neuropathy, your body may take longer to heal after surgery. In these cases, your surgeon might recommend more conservative approaches first or tailor your aftercare plan to prevent complications.
Foot Shape and Biomechanics
Certain foot shapes—like flat feet or high arches—can increase your risk of developing Morton’s neuroma in the first place. Even after surgery, if your foot’s structure isn’t addressed, the problem could return in the future. This is why custom orthotics or ongoing physical therapy may play a role in your long-term care.
Your Activity Level and Lifestyle
If you’re a runner, athlete, or someone who spends hours on your feet, your recovery might need extra care and patience. Returning to high-impact activities too soon can stress the healing tissues and cause setbacks. Your care team should work with you to balance rest and gradual return to movement based on your lifestyle goals.
Psychological and Emotional Considerations
It’s natural to feel anxious about foot surgery—especially if you’ve never had surgery before. Many patients worry about:
- How much pain they’ll have after surgery
- Whether the results will be worth it
- How long they’ll be off their feet
If any of these thoughts are on your mind, you’re not alone. Your foot specialist should walk you through what to expect step by step, so you feel confident and prepared.
Alternatives to Surgery for Severe Cases
Surgery isn’t the only option—even for severe cases of Morton’s neuroma. If you’re not ready for an operation, there are still advanced treatments worth exploring.
Cryotherapy (Cryoablation)
Cryotherapy uses extremely cold temperatures to freeze and shrink the inflamed nerve tissue. It’s minimally invasive and can be done under local anesthesia. Some studies suggest it offers meaningful relief for up to 70% of patients (source: Journal of the American Podiatric Medical Association).
Alcohol Injections (Neurolytic Injections)
This treatment involves injecting a high-concentration alcohol solution directly into the neuroma. The alcohol gradually breaks down the nerve, reducing pain over a series of sessions.
While results vary, some patients find it gives them enough relief to delay or avoid surgery entirely. This may work best if your neuroma is moderate to severe but not yet advanced enough to require removal.
Radiofrequency Ablation (RFA)
RFA uses heat energy delivered through a thin needle to disrupt the nerve’s ability to send pain signals. It’s a quick procedure, done under local anesthesia, and has shown promising results in patients who prefer non-surgical approaches (source: Foot and Ankle Clinics).
Combining Multiple Treatments
In some cases, combining treatments—like alcohol injections followed by custom orthotics or cryotherapy combined with physical therapy—can offer better results than using one method alone.
Conclusion
Deciding if and when to have surgery for Morton’s neuroma can feel overwhelming—but you don’t have to figure it all out on your own. Whether you’ve been struggling with foot pain for months, or you’re just starting to explore your options, the right treatment plan exists for you.
Surgery can provide lasting relief, especially if your neuroma is severe, but it’s not the only solution. Many patients find success with a combination of conservative treatments and newer minimally invasive techniques. The key is understanding your options and working with a specialist who listens to your concerns and tailors care to your unique needs.
If you’re ready to take the next step toward pain relief, consider booking a consultation with an experienced foot and ankle specialist. Together, you can build a plan that gets you back to the activities—and the life—you love.

If you’ve been struggling with persistent foot pain, especially in the ball of your foot, you may have already heard of Morton’s neuroma. It’s a common yet frustrating condition that can make every step uncomfortable.
But when does this condition need surgery? Is it possible to avoid surgery altogether? These are the questions many people ask after months of trying to manage their symptoms.
In this guide, we’ll walk you through everything you need to know—starting from what Morton’s neuroma actually is to how doctors diagnose it, and ultimately, the key indicators that show surgery might be the best option for you.
Understanding Morton’s Neuroma
What Exactly is Morton’s Neuroma?
Morton’s neuroma is a thickening of the tissue around the nerves leading to your toes—most often between the third and fourth toes. This thickened tissue compresses the nerve, leading to pain, tingling, or a burning sensation.
What Causes It?
There isn’t always a single cause, but several factors can put extra pressure on the forefoot, such as:
- Wearing tight or high-heeled shoes
- Participating in high-impact sports like running
- Having foot deformities such as flat feet, bunions, or hammertoes
Symptoms You Shouldn’t Ignore
Morton’s neuroma symptoms often start gradually but worsen over time if untreated. The most common complaints include:
- A feeling like you’re standing on a pebble or fold in your sock
- Sharp, burning pain in the ball of the foot
- Numbness or tingling in the toes
Why It Matters
Ignoring these symptoms can lead to long-term nerve damage, making treatment more difficult. That’s why understanding your condition early—and knowing when to escalate to more serious treatments—is critical.
Diagnostic Process
Step 1: Clinical Examination
Your journey to diagnosis usually starts with a physical exam. A foot specialist will press on the area between your toes to check for tenderness, a telltale “clicking” sensation (Mulder’s click), or reproduction of your pain.
Step 2: Reviewing Your Symptoms and History
Your doctor will ask questions like:
- When did the pain start?
- What makes it better or worse?
- What kind of shoes do you normally wear?
- Do you participate in sports that stress your feet?
This conversation helps connect the dots between your lifestyle and your symptoms.
Step 3: Imaging Tests
If needed, your doctor may order tests to rule out other conditions like stress fractures or arthritis. The most common imaging options are:
- Ultrasound: Shows soft tissue thickening around the nerve.
- MRI: Provides detailed images to confirm nerve enlargement.
Why an Accurate Diagnosis Matters
Some foot conditions mimic Morton’s neuroma, from capsulitis to metatarsalgia, so accurate diagnosis ensures you get the right treatment plan. Surgery isn’t even on the table until all other causes have been ruled out—and only if your pain continues despite trying conservative treatments.
Conservative Treatments and Their Role
If you’ve recently been diagnosed with Morton’s neuroma, surgery might sound intimidating. The good news is, surgery isn’t the first step in treatment—and for many people, it’s not needed at all.
Conservative treatments are non-surgical options designed to ease your symptoms and help you walk comfortably again. They focus on reducing pressure on the nerve, calming inflammation, and improving how your foot functions.
Footwear Modifications: Small Change, Big Impact
The shoes you wear play a major role in either relieving or worsening your pain. Narrow or high-heeled shoes squeeze the bones of your foot together, trapping the nerve between them.
Switching to wide, supportive shoes with low heels and plenty of cushioning can significantly reduce pressure on the affected nerve. Many people see real improvement with this one simple change.
Custom Orthotics and Padding
If changing your shoes isn’t enough, custom orthotics—specially made inserts that support your arch and redistribute weight—can help. Padding placed near the ball of your foot can also lift and separate the bones, reducing nerve compression.
Physical Therapy
A skilled physical therapist can guide you through stretches and exercises to ease tension in your foot and improve alignment. In some cases, poor foot mechanics contribute to nerve compression, and addressing that can provide lasting relief.
Medications and Injections
- Anti-inflammatory medications (like ibuprofen) can reduce swelling around the nerve.
- If pain is more severe, your doctor may suggest corticosteroid injections, which deliver targeted relief directly to the problem area.
Why Conservative Care Matters
Conservative treatments allow you to stay active while addressing the root cause of your symptoms. They’re also far less risky than surgery. Most experts recommend trying these approaches for several months before even considering surgery (source: American Orthopaedic Foot & Ankle Society).
When Conservative Treatments Fail
How Do You Know It’s Time to Re-evaluate?
For many people, conservative treatments bring relief—but not always. If you’ve given these options a fair try (typically 3-6 months) and your pain is still interfering with daily life, it may be time to explore other options.
Key Signs That Conservative Care Isn’t Working
- Ongoing pain despite footwear changes and orthotics
- Temporary relief from injections—but pain always returns
- Symptoms are getting worse over time
- You’ve had to significantly limit your activity to avoid pain
What’s Next?
When non-surgical care doesn’t bring enough relief, it’s natural to feel frustrated—or even worried about what comes next. This is where a thorough reassessment with your foot specialist becomes essential.
They’ll review your symptoms, check for any changes on imaging, and talk through the pros and cons of surgery or alternative treatments. Many people feel reassured when they realize that surgery, when needed, can be extremely effective at providing lasting relief.
Key Indicators That Surgery May Be Needed
Surgery Isn’t the First Step—But Sometimes It’s the Right One
The decision to have surgery for Morton’s neuroma isn’t made lightly. Most doctors recommend surgery only after conservative treatments have failed and your quality of life is suffering.
If you’re wondering whether you’ve reached that point, here are key indicators that surgery may be the next logical step:
1. Severe, Persistent Pain Despite Treatment
If you’ve diligently followed all the recommended treatments—changed shoes, tried orthotics, completed physical therapy, and even had injections—but the pain still limits your daily activities, surgery may offer the lasting relief you need.
2. Pain Is Limiting Your Mobility and Lifestyle
Are you avoiding walks, skipping workouts, or even limiting social activities because of foot pain? When pain starts controlling your life, it’s a clear sign that more aggressive treatment might be necessary.
3. Imaging Shows Progressive Changes
If follow-up imaging (like ultrasound or MRI) shows that the neuroma is getting larger or that the tissue is thickening even more, this can indicate that the nerve is under constant stress. Surgery may be the best way to remove the source of pain before it worsens further.
4. Recurrent Symptoms After Temporary Relief
Some people find relief with steroid injections, but if the pain keeps coming back and the relief periods are getting shorter, that’s a strong sign that injections are only masking the underlying problem, not solving it.
5. You Want a Long-Term Solution
If you’ve been managing symptoms for years and feel like you’re stuck in an endless cycle of flare-ups and treatment, surgery can offer a more definitive solution. While no procedure guarantees perfection, many patients experience significant, lasting relief after surgery.
What Surgery Can—and Can’t—Do
Surgery can remove or decompress the nerve, resolving the mechanical compression causing your pain. However, it does come with risks like numbness in the toes or possible recurrence of symptoms.
This is why it’s so important to work closely with a foot specialist who understands your specific goals—whether that’s returning to high-impact sports or simply being able to walk comfortably again.
Types of Surgical Options for Morton’s Neuroma
When conservative treatments have failed and your pain is affecting your quality of life, your doctor might suggest surgery for Morton’s neuroma. Surgery can sound daunting, but understanding your options can help you feel more confident about your decision.
Neurectomy: Removing the Problem Nerve
This is the most common surgery for Morton’s neuroma. In a neurectomy, the surgeon removes the thickened, damaged nerve between your toes. Without the nerve, the pain signals stop—but this also means you may experience some permanent numbness in the affected toes.
For many people, this trade-off is worth it if it means they can walk without pain again. According to research published in The Journal of Foot and Ankle Surgery, neurectomy success rates range between 75% to 85%, making it a reliable option when non-surgical treatments fail.
Nerve Decompression: Relieving Pressure Without Removing the Nerve
Some surgeons prefer a less aggressive approach—nerve decompression. Instead of removing the nerve, the surgeon releases the tight ligaments or tissue that’s pressing on it. This preserves the nerve and reduces the risk of numbness.
This technique may be more suitable if your neuroma is smaller or caught earlier. However, for chronic cases where the nerve is severely damaged, decompression might not offer long-term relief.
Open vs. Minimally Invasive Surgery
Both neurectomy and decompression can be done using either:
- Open surgery: A larger incision for direct access to the nerve.
- Minimally invasive surgery: Tiny incisions with specialized tools and sometimes a camera for guidance.
Minimally invasive techniques may offer faster recovery and less scarring, but they aren’t always suitable for larger neuromas. Your foot surgeon will recommend the approach that best fits your situation.
Risks and Benefits of Surgery
It’s natural to feel hesitant about foot surgery. Understanding both the potential benefits and the risks helps you make an informed choice.
What You Stand to Gain
- Significant pain relief: For most people, surgery successfully removes or relieves nerve pressure, offering lasting relief.
- Return to normal activity: Many patients can resume walking, sports, and daily routines once healing is complete.
- Permanent fix for some: When the nerve is removed, the source of the pain is gone for good.
What You Need to Consider
- Numbness: If the nerve is removed, the space between your toes may feel permanently numb. While this is usually not bothersome, it’s important to know.
- Scar tissue formation: In some cases, the healing process can create scar tissue that irritates the surrounding area—a condition called stump neuroma.
- Incomplete relief: While surgery helps the majority of patients, about 15-20% still experience some degree of pain afterward, especially if there are other underlying foot issues (like poor foot mechanics or arthritis).
Personal Factors That Affect Your Risk
- Your overall health (diabetes, poor circulation, or smoking can slow healing)
- Your activity level (athletes may need special recovery plans)
- Previous foot surgeries or chronic foot deformities
The Bottom Line
Surgery is a tool—not a magic fix. But when conservative care isn’t enough, it can give you back the ability to walk, move, and live without constant pain. Many patients say they wish they hadn’t waited so long to explore it.
Post-Surgery Recovery and Long-Term Outlook
If you’re considering surgery, you’re probably wondering: How long will recovery take? and What should I expect after surgery? Let’s break it down into clear phases so you can prepare confidently.
Immediate Post-Surgery: The First Few Days
After surgery, your foot will be bandaged and possibly in a surgical shoe to protect the area. You’ll need to keep your foot elevated and avoid putting weight on it for at least a few days.
Mild pain, swelling, and bruising are completely normal, and your doctor will recommend pain medication to keep you comfortable.
Early Healing: Weeks 1-3
You’ll gradually transition to walking short distances, often with the help of crutches or a walker. Many patients can wear comfortable, wide shoes after about 2-3 weeks, but high-impact activities are off-limits for a bit longer.
Full Recovery Timeline
- Walking comfortably: 4-6 weeks
- Return to most daily activities: 6-8 weeks
- High-impact sports or running: Around 3 months (or more, depending on healing)
Recovery speed varies from person to person. Factors like your age, weight, overall health, and how well you follow post-op care all play a role.
What Long-Term Results Can You Expect?
The good news is that the majority of patients experience substantial or complete pain relief after surgery. In fact, studies show that 80% or more of patients are satisfied with their outcome (source: Foot and Ankle International Journal).
However, some may notice:
- Mild numbness between the toes (usually not bothersome)
- Occasional stiffness if scar tissue forms
- Need for ongoing footwear adjustments to prevent new foot issues
Tips for Long-Term Foot Health
- Stick with supportive, well-cushioned shoes
- Use custom orthotics if your foot shape or gait needs correction
- Avoid repetitive stress from high-impact sports if possible
Special Considerations
Every foot is unique, and so is every case of Morton’s neuroma. Before deciding on surgery, it’s important to consider factors that could affect your outcome, recovery, and long-term comfort.
Your Overall Health and Medical History
If you have diabetes, poor circulation, or nerve conditions like neuropathy, your body may take longer to heal after surgery. In these cases, your surgeon might recommend more conservative approaches first or tailor your aftercare plan to prevent complications.
Foot Shape and Biomechanics
Certain foot shapes—like flat feet or high arches—can increase your risk of developing Morton’s neuroma in the first place. Even after surgery, if your foot’s structure isn’t addressed, the problem could return in the future. This is why custom orthotics or ongoing physical therapy may play a role in your long-term care.
Your Activity Level and Lifestyle
If you’re a runner, athlete, or someone who spends hours on your feet, your recovery might need extra care and patience. Returning to high-impact activities too soon can stress the healing tissues and cause setbacks. Your care team should work with you to balance rest and gradual return to movement based on your lifestyle goals.
Psychological and Emotional Considerations
It’s natural to feel anxious about foot surgery—especially if you’ve never had surgery before. Many patients worry about:
- How much pain they’ll have after surgery
- Whether the results will be worth it
- How long they’ll be off their feet
If any of these thoughts are on your mind, you’re not alone. Your foot specialist should walk you through what to expect step by step, so you feel confident and prepared.
Alternatives to Surgery for Severe Cases
Surgery isn’t the only option—even for severe cases of Morton’s neuroma. If you’re not ready for an operation, there are still advanced treatments worth exploring.
Cryotherapy (Cryoablation)
Cryotherapy uses extremely cold temperatures to freeze and shrink the inflamed nerve tissue. It’s minimally invasive and can be done under local anesthesia. Some studies suggest it offers meaningful relief for up to 70% of patients (source: Journal of the American Podiatric Medical Association).
Alcohol Injections (Neurolytic Injections)
This treatment involves injecting a high-concentration alcohol solution directly into the neuroma. The alcohol gradually breaks down the nerve, reducing pain over a series of sessions.
While results vary, some patients find it gives them enough relief to delay or avoid surgery entirely. This may work best if your neuroma is moderate to severe but not yet advanced enough to require removal.
Radiofrequency Ablation (RFA)
RFA uses heat energy delivered through a thin needle to disrupt the nerve’s ability to send pain signals. It’s a quick procedure, done under local anesthesia, and has shown promising results in patients who prefer non-surgical approaches (source: Foot and Ankle Clinics).
Combining Multiple Treatments
In some cases, combining treatments—like alcohol injections followed by custom orthotics or cryotherapy combined with physical therapy—can offer better results than using one method alone.
Conclusion
Deciding if and when to have surgery for Morton’s neuroma can feel overwhelming—but you don’t have to figure it all out on your own. Whether you’ve been struggling with foot pain for months, or you’re just starting to explore your options, the right treatment plan exists for you.
Surgery can provide lasting relief, especially if your neuroma is severe, but it’s not the only solution. Many patients find success with a combination of conservative treatments and newer minimally invasive techniques. The key is understanding your options and working with a specialist who listens to your concerns and tailors care to your unique needs.
If you’re ready to take the next step toward pain relief, consider booking a consultation with an experienced foot and ankle specialist. Together, you can build a plan that gets you back to the activities—and the life—you love.

Recent Posts
When is Surgery Needed for Morton’s Neuroma? Key Indicators
When is Surgery Needed for Morton’s Neuroma? If you’ve been struggling with persistent foot pain, especially in the ball of
