Is Morton's Neuroma Surgery Worth It? Pros and Cons
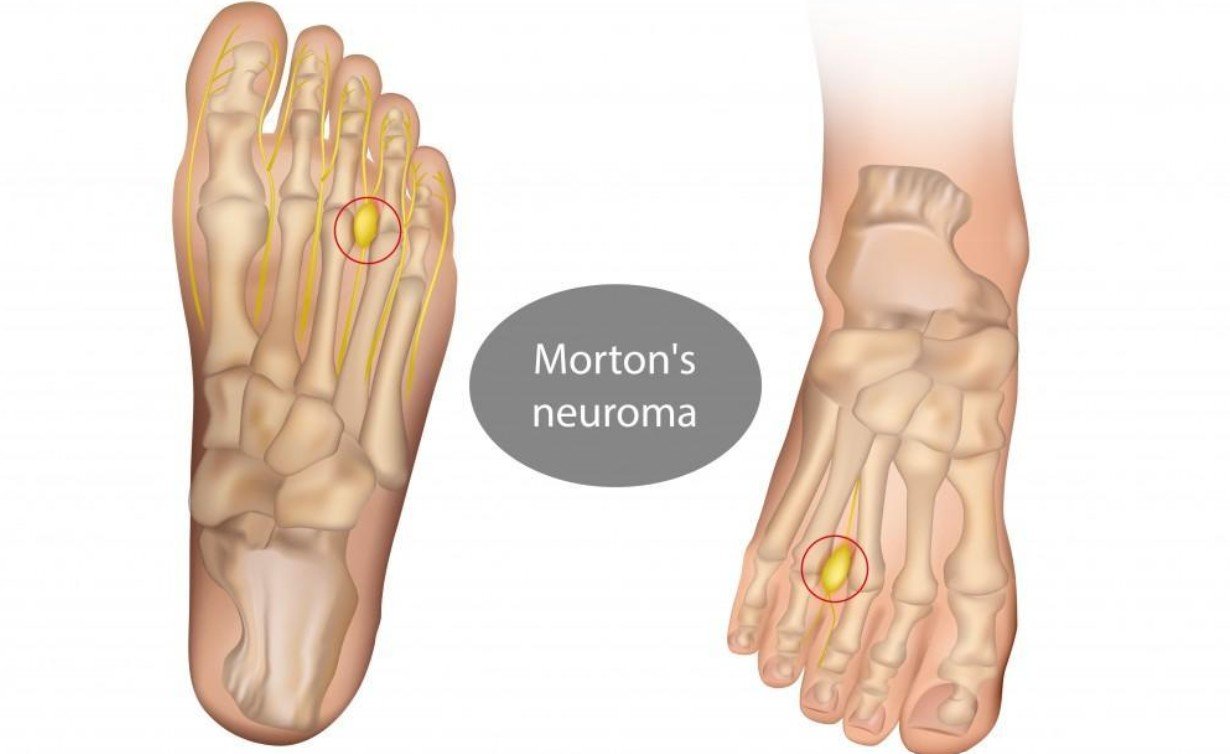
If you’ve been living with that sharp, burning pain between your toes, you’ve probably heard the term Morton’s Neuroma. It’s that frustrating condition where a nerve in your foot gets thickened and inflamed, making every step feel like you’re walking on a pebble.
When nothing else seems to work—changing shoes, trying injections, or even resting—surgery starts to sound like the final option. But before you go down that road, it’s natural to wonder: Is Morton’s Neuroma surgery actually worth it?
In this guide, we’ll walk through everything you need to know—from how the surgery works to real pros and cons—so you can make a confident, informed choice.
Understanding Morton’s Neuroma Surgery
What Happens During Morton’s Neuroma Surgery?
Morton’s Neuroma surgery is designed to relieve the pain caused by the thickened nerve in your foot. Depending on the severity and your specific case, surgeons may either:
- Remove the damaged nerve completely (called a neurectomy).
- Release pressure around the nerve by cutting nearby ligaments (called decompression surgery).
- In some cases, cryosurgery is used—a technique that freezes the nerve to stop it from sending pain signals.
How Long Does Surgery and Recovery Take?
The surgery itself is usually quick—often under an hour—but recovery can take weeks or even months. Most people are back to light walking in 2-3 weeks, but full recovery might take longer if your foot needs to rebuild strength or if scar tissue forms.
Who is a Candidate for Surgery?
Doctors typically recommend surgery if:
Why Do People Consider Surgery for Morton’s Neuroma?
When Nothing Else Works
Most people turn to surgery only after exhausting other options. If you’ve already tried:
- Changing to wider, supportive shoes
- Custom orthotics
- Steroid injections
- Physical therapy
…and the pain is still ruling your life, surgery might feel like the last hope.
Severe, Constant Pain
For some, Morton’s Neuroma isn’t just annoying—it’s debilitating. Walking to the store or standing at work becomes unbearable. When pain limits your ability to work, exercise, or even enjoy time with friends, surgery can feel worth the risk.
Impact on Quality of Life
It’s not just about pain—it’s about freedom. Many patients say Morton’s Neuroma robs them of their hobbies, social life, and independence. Surgery offers a potential way to regain that freedom, which is why some feel it’s worth it—even with the risks.
Benefits of Morton’s Neuroma Surgery (Pros)
Why Consider Surgery in the First Place?
If you’ve been living with Morton’s Neuroma for months or even years, you know how frustrating that sharp, burning pain can be. Simple things like walking barefoot, standing at work, or wearing your favorite shoes become impossible. When conservative treatments like orthotics, steroid injections, or physical therapy stop helping, surgery can start to feel like your last chance at relief.
Potential for Long-Term Pain Relief
For many patients, surgery can offer permanent pain relief—especially if the damaged nerve is removed entirely. Studies suggest that up to 80% of patients report significant or complete improvement after surgery (source: American Orthopaedic Foot & Ankle Society).
Regain Your Mobility and Active Life
Chronic foot pain doesn’t just hurt—it limits your freedom. Surgery can allow you to walk, exercise, and enjoy daily activities again without constantly thinking about your feet.
One Procedure, Long-Term Solution
Compared to repeated steroid injections or ongoing physical therapy, surgery is often a one-and-done solution. Some patients find comfort in knowing they won’t have to chase temporary fixes anymore.
May Reduce Dependency on Medication
If you’ve been relying on painkillers just to get through the day, surgery could help you cut back on medications—reducing the risk of long-term side effects.
Risks and Downsides of Morton’s Neuroma Surgery (Cons)
Surgery Isn’t a Guaranteed Fix
While many patients experience relief, some still have pain after surgery—or develop a new type of pain caused by scar tissue. In rare cases, the nerve can grow back abnormally (called a stump neuroma), creating a whole new problem.
Numbness and Sensory Changes
Depending on the type of surgery, you may lose sensation in part of your foot permanently. For some, this numbness is mild and manageable. For others, it’s unsettling—especially if you enjoy activities like barefoot yoga or dancing.
Recovery Can Be Longer Than Expected
While some people bounce back quickly, others find that swelling, stiffness, and discomfort linger for months. If your job requires you to be on your feet, this can be a significant drawback.
Risk of Infection or Surgical Complications
As with any surgery, there’s always a risk of infection, poor healing, or complications. People with diabetes, poor circulation, or other health conditions may face higher risks in this area.
Financial and Emotional Costs
Even if your insurance covers part of the procedure, surgery comes with additional costs—time off work, follow-up care, and potentially physical therapy to regain full mobility.
Cost Considerations
What Does Morton’s Neuroma Surgery Cost?
The cost of Morton’s Neuroma surgery can vary widely based on your location, the type of procedure, and whether you have insurance. In the U.S., surgical costs typically range from $3,000 to $7,000 (source: Healthline). If you need specialized procedures like cryosurgery, costs could be higher.
What’s Covered by Insurance?
Many insurance plans cover Morton’s Neuroma surgery if it’s deemed medically necessary—which usually means you’ve already tried conservative treatments without success. However, deductibles, copays, and out-of-pocket costs can still add up, especially if your plan has high surgical deductibles.
Additional Expenses to Plan For
Beyond the surgery itself, you might need to budget for:
- Pre-surgical consultations and imaging (like MRIs)
- Post-surgery checkups
- Physical therapy if your foot needs rehab
- Special shoes or orthotics to support your recovery
Comparing to Non-Surgical Options
It’s also helpful to compare these costs to non-surgical treatments. Custom orthotics, steroid injections, and physical therapy can add up over time. If you’ve already spent thousands on temporary fixes, investing in surgery for long-term relief might actually save money in the long run.
Recovery Process: What to Expect After Surgery
The First Few Days: What You’ll Experience
The first 24-48 hours after Morton’s Neuroma surgery are usually the most uncomfortable. Your foot will likely be swollen, tender, and bandaged, and you’ll need to stay off it as much as possible. Many surgeons recommend elevating your foot and using ice packs to control swelling.
You may be given pain medication, but some patients find they only need it for a couple of days. The goal during this phase is simple: rest and protect your foot.
Walking Again: What’s the Timeline?
Most people can start light walking within a few days, though you’ll need to wear a surgical shoe or protective boot for several weeks. Full weight-bearing walking often resumes within 3-4 weeks, but this varies depending on your specific procedure and how quickly your body heals.
Physical Therapy: Rebuilding Strength and Flexibility
In many cases, your doctor may recommend physical therapy to help your foot regain strength and mobility. Therapy might involve:
- Gentle stretching exercises to restore flexibility
- Balance training to prevent compensating injuries
- Massage or scar management if tissue stiffness becomes an issue
Possible Setbacks: Be Prepared for Bumps in the Road
Recovery isn’t always perfectly smooth. Some patients experience lingering swelling for months or develop scar tissue discomfort. Others feel numbness in the surgical area, which is normal but can feel strange at first.
The Full Recovery Picture
On average, patients return to regular activity between 6 and 12 weeks after surgery. If you have a physically demanding job or love intense activities like running, your timeline could be a bit longer. The key is to listen to your body and follow your surgeon’s advice closely.
Alternatives to Surgery: Exploring Non-Surgical Treatments
Why Explore Non-Surgical Options First?
Before jumping into surgery, most doctors recommend exhausting conservative treatments first—and for good reason. Many patients find they can manage or even eliminate their symptoms without surgery, especially if they catch Morton’s Neuroma early.
Orthotics and Footwear Modifications
Custom orthotics are often the first line of defense. These specially designed inserts redistribute weight in your foot, reducing pressure on the neuroma. Wearing shoes with a wide toe box and avoiding high heels can also make a noticeable difference.
Corticosteroid Injections: Temporary Relief
For moderate pain, your podiatrist may suggest corticosteroid injections. These can provide weeks or months of relief by reducing inflammation. However, results vary—some people get excellent results, while others see little improvement.
Alcohol Sclerosing Injections: A Lesser-Known Option
Another injectable option involves alcohol sclerotherapy, where a small amount of alcohol is injected directly into the neuroma. This works by shrinking the nerve tissue over time. It’s not as well-known as steroids, but some studies show promising results.
Physical Therapy: More Than Just Exercises
A skilled physical therapist can help correct foot mechanics, improve flexibility, and teach you nerve-friendly movement patterns. Combined with proper footwear, this can reduce pain triggers in your daily routine.
Shockwave Therapy: Non-Invasive Technology
Some clinics now offer shockwave therapy, where sound waves are applied to the foot to stimulate healing and break up scar tissue. While research is still evolving, some patients report pain relief after several sessions.
Lifestyle Changes: Small Shifts That Matter
Finally, simple adjustments to your lifestyle can go a long way. Maintaining a healthy weight reduces overall foot pressure, and choosing cushioned, supportive shoes can make every step more comfortable.
Real Patient Experiences and Testimonials
The Success Stories: Finding Relief After Surgery
Many patients who undergo Morton’s Neuroma surgery describe it as life-changing. They talk about finally being able to walk pain-free, wear their favorite shoes again, or return to activities they thought they’d lost forever.
One patient shared:
“Before surgery, even standing for 10 minutes felt unbearable. Now, I can hike with my kids again without thinking about my feet. It’s such a relief.”
The Mixed Experiences: Relief with Complications
Some patients experience partial relief but also encounter side effects—like numbness, scar tissue pain, or stiffness. While they are grateful the sharp nerve pain is gone, they still feel the surgery in their foot every day.
A common sentiment in this group is:
“The pain is better, but my foot doesn’t feel ‘normal’ anymore. I have some numbness, but it’s worth it compared to the constant stabbing pain before surgery.”
The Tougher Outcomes: Surgery Isn’t Always Perfect
There are also patients who regret the procedure—often due to stump neuroma, where the cut nerve regrows abnormally and causes new pain. For these individuals, surgery becomes the start of a new problem rather than the end of one.
One patient explained:
“I wish I’d tried more non-surgical treatments first. My pain came back six months after surgery, and now I’m dealing with nerve damage too.”
Key Takeaway: Every Foot (and Outcome) Is Different
What’s clear from these stories is that no two patients have the same journey. Surgery brings relief and risks—and understanding both sides is key to making the right choice for you.
Factors to Consider Before Choosing Surgery
Is Surgery the Right Choice for You?
Deciding whether to have Morton’s Neuroma surgery isn’t just about your foot—it’s about your whole lifestyle. Surgery can be effective, but it’s not the right path for everyone. Before making a decision, there are several key factors you’ll want to weigh.
How Severe Are Your Symptoms?
If you only feel pain occasionally, or if it’s manageable with wide shoes and rest, surgery may feel like an extreme step. On the other hand, if walking across the room feels like stepping on a pebble wrapped in fire, surgery might be worth considering.
What’s Your Lifestyle Like?
Think about how active you are and how important movement is to your daily life. If you’re a runner, hiker, or someone who’s constantly on your feet for work, persistent foot pain can dramatically affect your quality of life. In those cases, surgery may open the door to regaining your freedom.
Have You Tried Every Non-Surgical Option?
Most podiatrists recommend conservative treatments first—like custom orthotics, corticosteroid injections, or physical therapy. Surgery is usually a last resort, after less invasive options have failed. If you haven’t exhausted these, it’s worth exploring them before committing to surgery.
How Comfortable Are You with Surgical Risks?
Every surgery comes with risks—from infection to nerve damage. Some patients also develop stump neuroma, which is when the cut nerve regrows painfully. Understanding these risks upfront helps you make an informed decision, rather than facing unexpected surprises after the fact.
What’s Your Tolerance for Downtime?
While many people recover well from surgery, you will need time off your feet—especially in the first few weeks. If you have a demanding job or caregiving responsibilities, this recovery period might affect your decision.
In short: Surgery can be life-changing for some and frustrating for others. Knowing your personal goals, pain levels, and lifestyle needs can help you decide whether surgery fits into your bigger picture.
Expert Opinions: What Podiatrists and Surgeons Say
What Do Foot Specialists Really Recommend?
When you sit down with a podiatrist or foot surgeon, they won’t push surgery right away—and that’s a good thing. Experts follow a step-by-step approach, starting with the least invasive treatments before discussing surgery.
The Conservative Approach: Surgery is Rarely the First Step
The American College of Foot and Ankle Surgeons recommends starting with:
- Proper footwear adjustments (wide toe box, low heels)
- Custom orthotics to offload pressure
- Steroid injections to calm inflammation
- Physical therapy to improve foot function
Surgery typically only enters the conversation after 3-6 months of consistent non-surgical care with little to no improvement.
When Experts Recommend Surgery
Surgeons generally recommend surgery if:
- Your pain is severe and chronic.
- The neuroma is confirmed via imaging like ultrasound.
- Conservative treatments have failed.
- Your daily mobility and quality of life are seriously affected.
In these cases, a podiatric surgeon might explain surgical options—including neurectomy (removing the damaged nerve), decompression surgery (creating space around the nerve), or newer approaches like cryosurgery.
Advances in Surgical Techniques
The good news is that foot surgery has come a long way. Today’s procedures are often minimally invasive, meaning smaller incisions, faster healing, and lower risk of complications. Some surgeons even offer in-office procedures, which avoid the need for a hospital stay.
Experts Emphasize Realistic Expectations
One thing every experienced surgeon agrees on: surgery isn’t magic. While many patients get significant relief, not everyone becomes completely pain-free. Experts urge patients to weigh both benefits and risks carefully—and to ask plenty of questions before scheduling a procedure.
Comparing Surgical vs Non-Surgical Outcomes
Does Surgery Really Work Better?
One of the biggest questions you probably have is: Will surgery actually give me better results than non-surgical treatments? The answer depends on your specific case—but research gives us some helpful insights.
Pain Relief: Surgery vs Non-Surgical Care
- Studies show 70-85% of patients report significant pain relief after Morton’s Neuroma surgery.
- Non-surgical treatments can also provide good relief, especially when caught early—some reports show 50-60% success rates with orthotics and lifestyle changes alone.
- Patients with long-standing, severe neuromas tend to see better results from surgery than conservative care.
How Long Does Relief Last?
- Surgical relief can be long-lasting, especially if the neuroma is fully removed.
- Non-surgical relief is often temporary, especially if the root cause (like poor footwear) isn’t addressed.
- However, surgery comes with a risk of recurrence—especially if you return to activities that triggered the neuroma in the first place.
Quality of Life: What Patients Report
Patients who successfully recover from surgery often describe:
- Greater freedom of movement
- Ability to stand, walk, or exercise with much less pain
- Improved mental health—no longer dreading every step
On the non-surgical side, patients who find the right combination of treatments (like orthotics, injections, and therapy) also report good outcomes—but they often need ongoing care to maintain their results.
The Trade-Off: Invasiveness vs Convenience
- Surgery requires downtime, recovery, and surgical risks.
- Non-surgical options are low risk but may offer less predictable relief.
What the Data Says
In a 2022 study published in The Journal of Foot & Ankle Surgery, researchers found that patients who underwent surgery reported higher long-term satisfaction compared to those who only received non-surgical care. However, the rate of post-surgical complications—like numbness and stump neuroma—was about 10-15%.
Conclusion
Making the Right Choice for Your Foot Health
Choosing whether to have Morton’s Neuroma surgery is a deeply personal decision—and there’s no one-size-fits-all answer. If you’ve been struggling with burning pain, numbness, or that pebble-in-your-shoe sensation, it’s understandable to want relief as soon as possible.
Surgery can be a powerful solution, especially if non-surgical options haven’t worked for you. Many patients experience long-term pain relief after surgery, but it’s important to go in with realistic expectations. Recovery takes time, and like any medical procedure, surgery has its risks.
On the other hand, non-surgical treatments—like custom orthotics, physical therapy, and lifestyle changes—are often very effective, especially when started early. For some, these options provide enough relief to avoid surgery altogether.
What Matters Most: Your Quality of Life
Ultimately, the best choice is the one that fits your pain level, lifestyle, and personal comfort with risk. If you’re unsure where to start, a consultation with an experienced podiatrist can help you understand all your options and map out a personalized treatment plan.
Whether you choose surgery or stick with non-surgical care, the goal is the same: to help you walk comfortably, live fully, and regain control over your life.
FAQs
How do I know if I really need Morton’s Neuroma surgery?
Most podiatrists recommend surgery only after you’ve tried conservative treatments—like wearing wider shoes, using custom orthotics, and getting cortisone injections. If you’ve had persistent pain for several months and nothing else has worked, surgery might be worth considering.
What’s the success rate of Morton’s Neuroma surgery?
Studies show that 70-85% of patients experience significant pain relief after surgery. However, some patients develop complications like scar tissue or stump neuroma, so it’s important to discuss the full picture with your surgeon.
How long does recovery take after surgery?
Most people can start light walking within a few weeks, but full recovery—especially if you want to return to sports or strenuous activity—can take up to 3 months. Every case is different, and your overall health plays a big role in healing.
What are the risks of Morton’s Neuroma surgery?
Common risks include:
- Infection at the surgical site
- Nerve damage (leading to numbness or tingling)
- Development of a stump neuroma (painful nerve regrowth)
- Longer-than-expected recovery
That said, choosing a skilled, board-certified podiatric surgeon reduces your risk significantly.
Is surgery my only option if I want lasting relief?
Not at all. Many people find lasting relief with:
- Proper footwear (wide toe box, low heels)
- Custom orthotics to offload pressure
- Steroid injections to calm inflammation
- Physical therapy to improve foot strength and flexibility
If you respond well to these, you may never need surgery.
How much does Morton’s Neuroma surgery cost?
The cost can range from $3,000 to $10,000 or more, depending on your location, the type of surgery, and whether your insurance covers it. It’s always smart to check with your insurance provider and ask your clinic for a detailed cost breakdown before moving forward.
Can the neuroma come back after surgery?
In some cases, yes—especially if the root cause (like poor footwear or repetitive foot stress) isn’t addressed. That’s why post-surgery care—like proper shoes, orthotics, and gradual return to activity—is so important.
How do I choose the right podiatrist or surgeon?
Look for someone who:
- Specializes in foot and ankle surgery
- Has experience specifically with Morton’s Neuroma procedures
- Takes the time to explain both surgical and non-surgical options
- Comes recommended by trusted sources or credible medical associations.
Recent Posts
Is Morton’s Neuroma Surgery Worth It? Pros and Cons
Is Morton’s Neuroma Surgery Worth It? Pros and Cons If you’ve been living with that sharp, burning pain between your
