If you’ve had surgery for Morton’s neuroma, you’re probably hoping the pain is gone for good. But what happens if the discomfort creeps back months or even years later? This is a common fear for many people after foot surgery—and it’s a valid concern.
In this guide, we’ll explore the possibility of Morton’s neuroma recurrence after surgery, why it happens, and what you can do to lower the risk. Whether you’re preparing for surgery or recovering from one, understanding the recurrence risks can help you make informed decisions about your foot health.
What is Morton’s Neuroma?
A Quick Overview
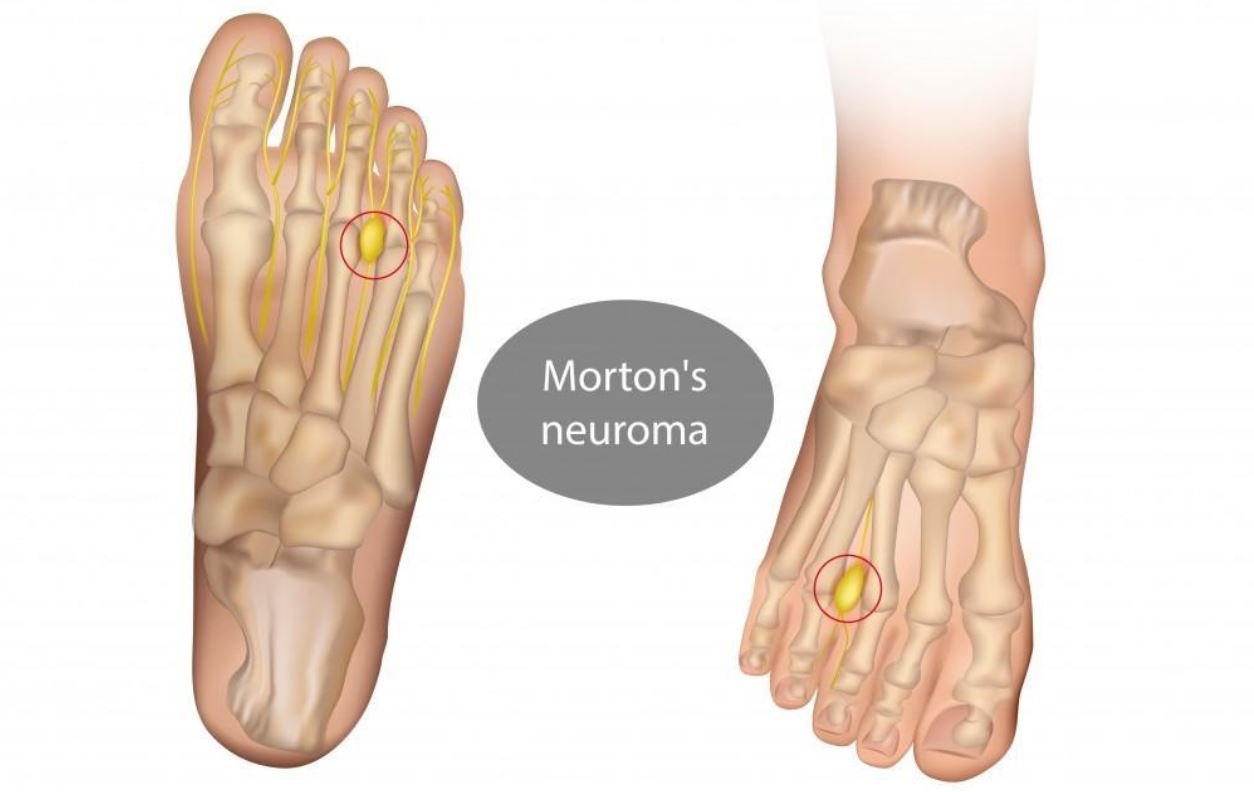
Morton’s neuroma is a painful condition affecting the nerves between the toes, most commonly between the third and fourth toes. It occurs when the nerve tissue thickens due to constant irritation, pressure, or injury. This thickening compresses the nerve, leading to sharp pain, burning sensations, and even numbness in the ball of the foot.
What Causes It?
Some common triggers for Morton’s neuroma include:
- Wearing tight or narrow shoes that squeeze the toes together.
- High-impact activities like running, which place repeated stress on the foot.
- Foot structure issues, such as flat feet, high arches, or abnormal toe alignment.
Common Symptoms
People with Morton’s neuroma often describe the sensation as:
- Feeling like a pebble is stuck under the ball of the foot.
- Burning pain radiating into the toes.
- Numbness or tingling between the toes.
Why Surgery Becomes Necessary
When conservative treatments like shoe changes, orthotics, and injections no longer provide relief, surgery becomes an option. Surgery can reduce the pressure on the nerve—or remove it entirely—to stop the pain.
Types of Surgery for Morton’s Neuroma
Surgical Approaches Explained
There are two main surgical procedures used to treat Morton’s neuroma:
1. Neurectomy (Nerve Removal)
In this procedure, the surgeon removes part of the affected nerve to eliminate the source of pain. While effective, removing the nerve can sometimes lead to stump neuroma, where the cut nerve forms a painful mass of scar tissue.
2. Decompression Surgery
This is a less invasive option, where the surgeon releases nearby structures (like tight ligaments) to reduce pressure on the nerve. This technique preserves the nerve rather than removing it. However, the risk of recurrence can be slightly higher if the underlying cause (such as faulty foot mechanics) isn’t addressed.
Choosing the Right Surgery for You
The best surgical option depends on several factors:
- Severity of your symptoms
- Your overall foot structure
- Your activity level and lifestyle
- Your surgeon’s experience and preference
Success Rates and What to Expect
Studies show that Morton’s neuroma surgery generally has a success rate of around 75-85%, but recurrence can happen—especially if post-surgery care isn’t carefully managed. Understanding these risks ahead of time can help you make more confident choices about your treatment.
What is Recurrence?
Understanding Recurrence in Morton’s Neuroma Surgery
If you’ve already had surgery for Morton’s neuroma, the last thing you want is for the pain to come back. Unfortunately, recurrence is a real possibility—and understanding what it means can help you prepare.
In simple terms, recurrence refers to the return of symptoms—like burning pain, numbness, or discomfort in the ball of your foot—after you’ve had surgery to treat Morton’s neuroma. This doesn’t always mean the neuroma itself has physically grown back. Sometimes, the pain stems from scar tissue, nerve regrowth, or even other underlying foot problems that weren’t fully addressed during surgery.
Is It True Recurrence or Something Else?
This is where things get tricky. Some patients experience persistent pain right after surgery, while others feel better for months or even years—only for the pain to gradually return. True recurrence means the nerve or surrounding tissue is once again causing compression or irritation. However, other issues like stump neuroma (a painful nerve ending at the surgical site) can mimic recurrence.
How Common is Recurrence After Surgery?
Recurrence Rates Explained
One of the biggest concerns people have after Morton’s neuroma surgery is: Will the pain come back? The truth is, recurrence isn’t rare, but it’s not guaranteed either. Research suggests that recurrence rates for Morton’s neuroma surgery range from 10% to 30%, depending on the type of surgery performed, surgical technique, and individual factors like your foot structure and lifestyle (NCI, 2023).
Factors That Influence Recurrence Rates
Some factors make recurrence more likely:
- Type of surgery: Nerve removal (neurectomy) tends to have lower recurrence rates than decompression surgery, but it carries other risks.
- Surgical technique: Experienced surgeons using updated techniques often see better long-term outcomes.
- Foot mechanics: If you have underlying issues like flat feet, high arches, or bunions—and they aren’t corrected—the same pressure that caused the neuroma in the first place could lead to new nerve irritation.
- Post-surgery care: Returning to narrow shoes or high-impact activities too soon after surgery can increase your risk.
Timeframe for Recurrence
Recurrence can happen at any point after surgery. Some people experience it within a few months, while others feel fine for years before symptoms return. This unpredictable timeline is one of the frustrating realities for many patients.
Causes of Recurrence After Surgery
Why Does Morton’s Neuroma Come Back?
Recurrence isn’t always caused by a surgeon’s mistake. In fact, there are several reasons why symptoms can return, even after a successful procedure. Understanding these causes can help you spot risk factors before surgery or address potential problems after surgery.
Common Causes of Recurrence
Here are the key reasons recurrence happens:
- Incomplete removal of the nerve: In neurectomy procedures, if the entire affected nerve segment isn’t removed, some tissue left behind can continue to cause symptoms.
- Nerve regrowth and stump neuroma: When a nerve is cut during surgery, it can sometimes form a painful lump of scar tissue at the end (stump neuroma). This lump can irritate surrounding tissue, leading to similar symptoms as the original neuroma.
- Scar tissue formation: Surgery itself triggers scar formation. In some cases, this scar tissue presses on nearby nerves, recreating the same burning or tingling sensations.
- Incorrect initial diagnosis: Occasionally, foot pain diagnosed as Morton’s neuroma could be caused by a different issue (like tarsal tunnel syndrome or metatarsalgia). If surgery was performed based on an incorrect diagnosis, the real problem remains—leading to continued pain.
- Foot mechanics and footwear: If you continue to wear tight, narrow shoes or put excessive stress on your forefoot after surgery, the same compressive forces could irritate other nerves, leading to new neuroma formation in nearby toes.
Recurrence or New Neuroma?
In some cases, what feels like recurrence could actually be a brand-new neuroma forming in a different location, especially if biomechanical issues (like poor arch support or gait problems) were never corrected.
Psychological Factors and Nerve Sensitivity
It’s also important to recognize that chronic pain itself rewires how your brain processes foot sensations. After surgery, some patients develop heightened nerve sensitivity—meaning even minor irritation triggers significant pain. This isn’t true recurrence, but it feels just as real.
Symptoms of Recurrent Morton’s Neuroma
What Does Recurrence Feel Like?
If you’ve undergone surgery for Morton’s neuroma, you probably remember the burning pain or sharp, stabbing sensations in the ball of your foot. When symptoms start creeping back, it’s natural to wonder—is this the neuroma returning?
Recurrent Morton’s neuroma doesn’t always feel identical to your pre-surgery pain, but many patients describe similar discomfort, including:
- A burning or tingling sensation between the toes.
- A sharp, shooting pain that radiates into the toes, especially while walking.
- The unsettling feeling of a pebble stuck under the foot, even when nothing is there.
- Increased sensitivity, where even light pressure causes pain.
- Occasional numbness in the toes after standing for long periods.
New Symptoms to Watch For
In some cases, recurrent neuroma pain may feel slightly different than before. This can happen if scar tissue or a stump neuroma (a painful nerve ending left after surgery) develops.
You may notice:
- Pain centered directly over the surgical scar.
- A tender lump under the ball of the foot.
- Pain triggered by certain shoes, especially those with narrow toe boxes.
- A deep, aching discomfort that gets worse as the day progresses.
Don’t Ignore Early Warning Signs
Catching symptoms early gives you more options for non-surgical treatment. If you’ve had surgery and start to notice even mild discomfort, it’s worth discussing with your specialist—before the pain takes over again.
Diagnosing Recurrent Morton’s Neuroma
Why Diagnosis Isn’t Always Straightforward
One of the biggest challenges with recurrent Morton’s neuroma is that the symptoms can overlap with other foot problems—like capsulitis, plantar plate tears, or even stress fractures. That’s why a thorough evaluation is essential.
Step 1: Your Symptom History
Your doctor will want to know:
- When your symptoms returned and how they compare to pre-surgery pain.
- What types of shoes you typically wear.
- Whether your symptoms improve with rest or worsen with activity.
- If you’ve made any recent changes to your footwear, activity level, or foot care routine.
Step 2: Physical Examination
Next, your foot specialist will gently press around the area where your neuroma was removed. They’ll check for:
- Tenderness directly over the nerve site.
- A noticeable lump (which could indicate scar tissue or stump neuroma).
- Toe splaying or shifting, which could suggest structural problems contributing to nerve irritation.
Step 3: Imaging Tests
In many cases, imaging is used to confirm the diagnosis. Depending on your symptoms, your doctor might recommend:
- Ultrasound: This is excellent for spotting nerve thickening, scar tissue, or fluid buildup.
- MRI: Useful for identifying both soft tissue changes and subtle nerve regrowth.
Step 4: Diagnostic Injections
If it’s unclear whether the pain is truly coming from a recurrent neuroma, a diagnostic nerve block may be used. This is where a small amount of anesthetic is injected around the nerve. If the pain disappears temporarily, it’s a strong clue that the nerve is the source.
Why Diagnosis Matters
The right diagnosis doesn’t just confirm recurrence—it helps guide your treatment options. For example, pain from scar tissue might respond to physical therapy, while true nerve regrowth may need a different approach.
Risk Factors for Recurrence
Who is Most at Risk?
If you’re wondering whether recurrence is avoidable, the answer is sometimes yes—but not always. Certain factors make recurrence more likely, and understanding these risks helps you make smarter choices both before and after surgery.
Surgical Risk Factors
Some recurrence risks relate directly to how the surgery was performed:
- Incomplete Nerve Removal: If part of the damaged nerve is left behind, it can still trigger pain.
- Nerve Regrowth: After nerve removal, the cut end can form a stump neuroma, which may become just as painful as the original condition.
- Scar Tissue Formation: Excessive scar tissue can press on neighboring nerves, recreating the same painful sensations.
Foot Anatomy and Biomechanics
Your foot structure plays a huge role in recurrence risk. If you have:
- Flat feet (which shift more pressure onto the forefoot).
- High arches (which focus pressure on the ball of the foot).
- Bunions or hammertoes (which crowd the toes).
These mechanical issues can continue to irritate the nerve, even after surgery.
Lifestyle and Footwear Choices
How you treat your feet after surgery also matters:
- Narrow, pointy shoes compress the toes, recreating the conditions that caused your neuroma in the first place.
- High heels shift your weight forward, increasing pressure on the ball of your foot.
- High-impact sports like running or jumping can re-irritate healing tissue.
Healing and Post-Surgery Care
Rushing back to normal activities before your foot is fully healed raises your risk, too. Proper physical therapy, custom orthotics, and smart footwear choices can significantly reduce the chance of recurrence.
Health and Healing Factors
Finally, your age, weight, and general health all play a role. People with diabetes or poor circulation may heal more slowly, increasing the chance of complications like scar tissue buildup.
Preventing Recurrence After Surgery
Why Prevention Matters After Morton’s Neuroma Surgery
If you’ve been through surgery once, the last thing you want is to face the pain again. Recurrence isn’t inevitable, but it’s a real risk—especially if the underlying causes of your neuroma aren’t fully addressed. The good news? There are steps you can take to protect your feet and lower your chances of recurrence.
Choose the Right Footwear
Your shoes play a massive role in either helping your foot heal or re-creating the same conditions that caused the neuroma in the first place. After surgery, you’ll want to:
- Wear shoes with a wide toe box that lets your toes spread naturally.
- Avoid high heels, which shift pressure onto the ball of your foot.
- Look for cushioned soles that absorb shock as you walk.
- Consider custom orthotics if your foot structure (like flat feet) contributed to the original problem.
Manage Foot Mechanics
If foot structure was part of the cause, surgery alone isn’t a full fix. Many podiatrists recommend physical therapy to improve foot strength and alignment, reducing pressure on the nerves between your toes. Simple exercises can strengthen your arch and improve your gait.
Gradual Return to Activity
Rushing back into high-impact exercise or long hours on your feet can irritate the healing tissues—increasing your risk of scar tissue buildup or nerve regrowth. Work with your specialist to ease back into normal activity, and listen to your body when it signals discomfort.
Regular Check-Ins
Even if you feel great after surgery, it’s smart to schedule routine follow-ups with your podiatrist. Catching small issues—like minor nerve irritation—early gives you more options to treat it conservatively before it worsens.
Many Patients Find Proactive Care Helpful
Some patients also benefit from periodic massage therapy, foot taping techniques, or offloading pads to protect sensitive areas. These aren’t cure-alls, but they can keep minor irritations from spiraling into full-blown recurrence.
Treatment Options for Recurrent Morton’s Neuroma
What If Your Symptoms Return?
If the pain creeps back after surgery, you’re not alone—and you’re not out of options. Recurrent Morton’s neuroma can be frustrating, but there are both conservative treatments and surgical revisions that can help you find relief again.
Non-Surgical Treatments
Before jumping into another surgery, most specialists recommend trying less invasive options first. These may include:
- Padding and offloading: Special pads or custom orthotics can help shift pressure off the sensitive area.
- Physical therapy: Strengthening your foot and improving gait mechanics may reduce nerve irritation.
- Injection therapy: Corticosteroid or alcohol injections may calm inflammation and reduce nerve sensitivity.
- Laser therapy: Some clinics offer low-level laser treatments, which can reduce pain and inflammation.
- Footwear modifications: Wearing wide, supportive shoes that don’t pinch your toes is critical in both prevention and treatment.
Revision Surgery: When Is It Needed?
If non-surgical treatments don’t bring relief, your specialist might discuss revision surgery. This is more complex than your first procedure, as the surgeon needs to address scar tissue, potential stump neuroma, and any unresolved biomechanical issues.
Revision Surgery Options
Depending on your case, revision surgery may involve:
- Removing any remaining nerve tissue.
- Addressing stump neuroma by removing the painful nerve ending.
- Releasing scar tissue to reduce nerve compression.
- Correcting structural issues (like bunions or flat feet) to prevent further irritation.
Many Patients Combine Treatments
Often, the most successful treatment plan blends several approaches—a mix of footwear changes, physical therapy, and targeted pain relief strategies. The key is creating a plan that works for your unique foot structure and lifestyle.
Psychological Impact of Recurrence
The Emotional Toll of Chronic Foot Pain
Living with foot pain—especially after you’ve already had surgery—can be incredibly discouraging. Many patients feel a mix of frustration, anxiety, and even guilt, wondering if they somehow caused the recurrence.
If you feel like no one understands how much this impacts your daily life, you’re not alone. Something as simple as standing in line or walking to your car can feel daunting, and the fear of pain returning after every step can be mentally exhausting.
The Cycle of Fear and Avoidance
It’s common for people with recurrent neuroma pain to avoid activities they used to enjoy—whether it’s walking with friends or working out. This avoidance often worsens your overall foot health, because inactivity can weaken your foot muscles, setting you up for even more mechanical problems.
You’re Not to Blame
One of the most important things to understand is that recurrence isn’t your fault. It’s often due to factors outside your control—like how your nerve heals, your natural foot shape, or scar tissue forming unexpectedly. Taking care of your feet is important, but self-blame only adds unnecessary stress.
Psychological Support Matters
If you’re struggling emotionally, reaching out to a pain psychologist or joining a support group can be incredibly helpful. Sharing your experience with others who’ve been through similar challenges can validate your feelings and help you build coping strategies.
Many Patients Find Hope Through Comprehensive Care
When patients combine physical care (like footwear changes and therapy) with emotional support and clear communication with their specialist, they often feel more in control of their recovery—and that sense of control itself can reduce fear and anxiety.
The First Step: Talk to Your Specialist
If you’re worried about recurrence—or you’re already noticing symptoms creeping back—you don’t have to figure this out alone. Many foot specialists offer second opinion consultations specifically for post-surgical patients, helping you explore your options without pressure.
Conclusion
What You Should Take Away
Facing the possibility of Morton’s neuroma recurrence after surgery can feel overwhelming, especially after going through the initial recovery. But understanding the risks—and more importantly, what you can do to reduce them—gives you back a sense of control.
Surgery is often effective, but it’s not a guaranteed one-time fix. Recurrence can happen, especially if underlying causes like poor foot mechanics or improper footwear aren’t addressed. However, with the right aftercare, regular monitoring, and a proactive approach to foot health, you can significantly lower your risk.
Stay Connected with Your Specialist
The most important thing is to stay in touch with your foot specialist, even after you’re feeling better. Catching small problems early—like minor nerve irritation—can often prevent them from becoming full-blown recurrence. If you ever notice familiar symptoms returning, don’t wait to seek advice.
You’re Not Alone in This Journey
If you’re feeling anxious about recurrence, you’re not alone—and you’re not out of options. Whether you need guidance on prevention strategies, conservative treatments, or even a second opinion, there are experts ready to help. Many patients find that a combination of medical care, lifestyle changes, and emotional support makes a huge difference in both recovery and long-term foot health.
FAQs
Can Morton’s neuroma really come back after surgery?
Yes, recurrence after Morton’s neuroma surgery is possible, though not everyone experiences it. Research suggests recurrence rates vary between 5% and 30%, depending on factors like surgical technique, scar tissue formation, and individual foot structure.
What does recurrent Morton’s neuroma feel like?
It often feels very similar to the original neuroma pain—a burning sensation, sharp stabbing pain, or the constant feeling of something stuck under the ball of your foot. Pain may worsen when walking, especially in narrow shoes.
Why does recurrence happen?
Recurrence can happen due to several reasons:
- Scar tissue: Thick scar tissue can irritate nearby nerves.
- Stump neuroma: A painful nerve ending forms where the neuroma was removed.
- Underlying foot mechanics: Issues like flat feet or tight footwear can recreate nerve compression.
- Incomplete nerve removal: In rare cases, a portion of the neuroma may remain.
How can I lower my risk of recurrence?
You can reduce your risk by:
- Wearing wide, supportive shoes with plenty of cushioning.
- Using custom orthotics if your foot shape needs extra support.
- Gradually returning to activity after surgery.
- Strengthening your foot muscles through physical therapy exercises.
- Scheduling regular follow-ups with your podiatrist.
Is revision surgery the only option if the neuroma comes back?
Not necessarily. Many patients respond well to non-surgical treatments, including:
- Corticosteroid or alcohol injections.
- Physical therapy to correct foot mechanics.
- Offloading pads to reduce nerve pressure.
- Laser therapy to ease pain and inflammation.
If conservative treatments don’t work, your specialist might recommend revision surgery, but that’s usually a last resort.
Should I worry about recurrence even if my surgery went well?
It’s always smart to be aware, but not every patient experiences recurrence. If you follow your specialist’s advice—wearing the right shoes, staying active in smart ways, and addressing any foot issues early—you greatly improve your chances of staying pain-free long-term.
